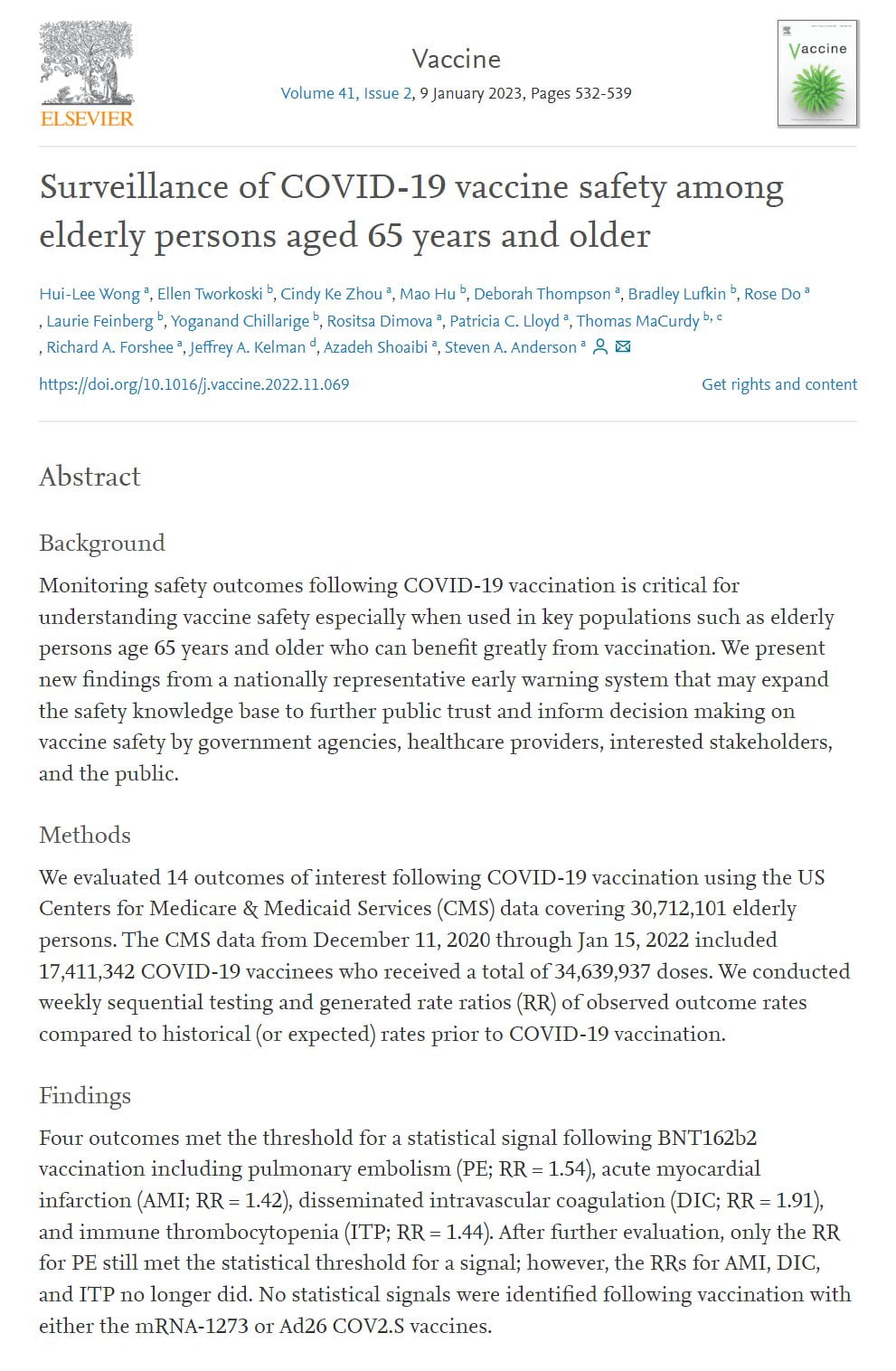
We show that the initially high mRNA vaccine-induced blood and salivary anti-S IgG levels, particularly IgG1, markedly decrease over time and approach the lower levels induced with the adenovirus-based vaccine.
All three vaccines induced, contrary to the short-term anti-S IgG1 response with high sialylation and galactosylation levels, a long-term anti-S IgG1 response that was characterized by low sialylation and galactosylation with the latter being even below the corresponding total IgG1 galactosylation level.
Instead, the mRNA, but not the adenovirus-based vaccines induced long-term IgG4 responses – the IgG subclass with inhibitory effector functions.
Furthermore, salivary anti-S IgA levels were lower and decreased faster in naïve as compared to pre-infected vaccinees.
Repeated immunization of naïve individuals with the mRNA vaccines increased the proportion of the IgG4 subclass over time which might influence the long-term Ab effector functions.
These data shed light on these novel vaccine formats and might have potential implications for their long-term efficacy.
mRNA vaccines against SARS-CoV-2 induce comparably low long-term IgG Fc galactosylation and sialylation levels but increasing long-term IgG4 responses compared to an adenovirus-based vaccine.
https://www.frontiersin.org/articles/10.3389/fimmu.2022.1020844/full?s=09#B75
IgG4 antibodies are non-neutralizing antibodies, akin to antibodies produced in response to allergies. Repeated immunization with mRNA vaccines sensitizes a long-term allergic response to COVID, leaving you more susceptible than you would otherwise have been.